Are there too many ID specialists?
As ID fellowship interview season begins, there have been some interesting posts on the program directors’ list serve. After last year’s historically awful match, program directors are looking for answers, and finding none. A longtime program director opined that “there are too many ID programs”, referring back to the famous words of Dr. Robert Petersdorf that we’ll eventually end up “culturing one another”. This individual argued that ID programs should drop their research emphasis and instead train fellows in the skill sets they’ll need in community practice (infection prevention, stewardship, clinical microbiology, basic business principles, etc.). Furthermore, the argument went, the reason IDSA has been slow to respond is that the society leadership is over-represented by academic ID physicians.
Now, it is objectively true that we have too many ID training programs when compared with the existing demand for training….but I frankly hadn’t considered the argument that we simply have too many training programs compared with actual future need for ID physician expertise. So I went back and pulled the piece in which Petersdorf made his argument that we are training too many ID docs. Interestingly, his argument about how ID programs should adapt to future needs was the exact opposite of that being proposed by the program director mentioned above. Petersdorf argued that:
“...the existence of specialists in most community hospitals will lead to fewer referrals to the teaching centers and the resulting lack of patients will lead training programs to atrophy. Infectious Disease is destined to function best as an academic specialty whose trainees should pursue careers primarily as investigators. The number of clinicians leaving training should be reduced and not further glut the marketplace; they should be based in academic divisions and devote their clinical time and effort to the care of complex referrals and to indigent patients.”
So which is it? Do we have too many training programs (and thus are counter-productively trying to gin up interest in ID when we don’t really need more ID docs)? Or are we destined to face a critical shortage of ID specialists in the near future?
In my view, the answer depends upon answers to other questions that the current trainee has very little control over, including: (1) will the funding climate improve for physician scientists?, (2) will health care reimbursement in the U.S. eventually move fully from RVU-based to value-based?, (3) if the answer to question 2 is yes, how will that health care be delivered?, and (4) will ID physicians continue to play a major role in individual hospital quality-safety programs (e.g. infection prevention, antimicrobial stewardship), or will their roles be supplanted by hospitalists and other non-ID trained quality-safety experts?
Expanding on questions 2 and 3 above, I’ve often heard it said that value-based purchasing and the move away from RVU-driven reimbursement would be a boon to ID docs. I’m not so sure about that. Many areas of our rural state have no local ID expertise—as a result, our faculty field several calls per day from providers seeking (free) ID expertise, are now performing “eConsults”, and plans are for us to greatly expand our telehealth programs. These programs are designed not, as Petersdorf envisioned, to increase “referrals to teaching hospitals”, but instead are meant to reduce the need for these expensive referrals.
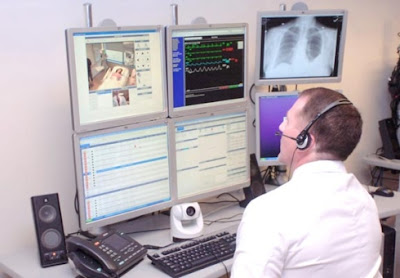
What is the least expensive way to provide ID expertise to a large population? Sadly, I envision a future “ID Command Center”: an advanced telehealth unit that allows one ID doc to provide consultative support to entire healthcare networks, providing instant access to all the required information….except for that which can be gained by actually touching the patient. Sorry, Abraham.
What do you all think?
Photo credit: Mike Staugaitis

I think we will see a "supply and demand" situation play out in the future. If our numbers go down and health care suffers because of that, then the compensation of the fewer ID physicians left will increase, which will then cause an increase in the number of residency applicants. However, if others fill in the gap of ID physicians then we will need to reinvent ourselves and adapt to the changing landscape. In addition to Quality related activities, Population Health is a field that needs people trained in epidemiology (with MPHs or MSc).
ReplyDelete