HAI surveillance definitions update: The good, the bad, and the ugly
First, the good: As of January 1, CDC has modified the definition for catheter associated urinary tract infection (CAUTI). This was sorely needed to improve specificity.
The new CAUTI definition can be found here and a video on the changes can be viewed here. In summary, there are 3 major changes:
- A positive culture requires >100,000 CFUs
- Yeast have been eliminated from the definition
- Urinalysis is no longer part of the definition
The new definition will better align with working clinical definitions used by physicians to diagnose and treat CAUTI.
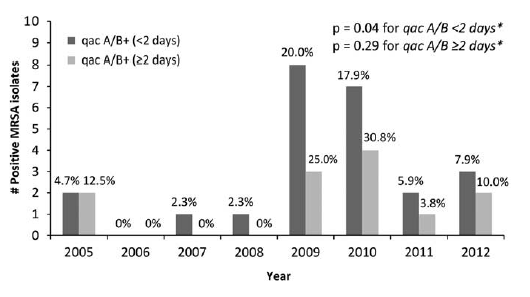
Now, the bad: Unfortunately, we still have the problem of CLABSI surveillance only allowing the denominator to include one central line per day even though more than one central line may be present. This punishes academic medical centers where the sickest patients receive care. A recent study in Infection Control and Hospital Epidemiology from the University of Rochester sheds some light on this issue. Investigators there performed a case control study to evaluate the risk of multiple central lines on development of CLABSI. They compared patients with 1 central line to those with more than 1. They found that even when controlling for chemotherapy, hemodialysis, use of TPN, length of stay, age, acute and chronic illness (using APACHE and Charlson indices, respectively), patients with more than 1 central line are 3.4 times more likely to develop CLABSI.
Finally, the ugly: Although CDC developed a definition for CLAMBI (central line associated mucosal barrier injury bloodstream infection) and hospitals are using it, these infections will still be publicly reported as CLABSIs. The end result is that hospitals with large populations of oncology patients are forced to report falsely elevated CLABSI rates. Since there is agreement that CLAMBI is not preventable and actually not causally associated with central lines, this situation is both ridiculous and harmful.
Over the past several weeks, there have been numerous reports in the media regarding hospitals penalized by CMS in the HAC reduction program. Interestingly, over half of the academic medical centers found themselves in the 25% of hospitals that were financially penalized. It's not surprising given that the cards are clearly stacked against them by the NHSN surveillance methodology. As the stakes get ever higher, the need for more precision in the methodology is imperative.

Comments
Post a Comment
Thanks for submitting your comment to the Controversies blog. To reduce spam, all comments will be reviewed by the blog moderator prior to publishing. However, all legitimate comments will be published, whether they agree with or oppose the content of the post.