something something antibiotics something something
It's been a crazy couple weeks out here on the edge of the prairie. Clinical service, grants, papers, holidays, Ebola?, the ESCMID-SHEA course in Phuket and SHEA2015 have swallowed up my fall. Get those SHEA abstracts ready folks - the deadline is fast approaching - January 16th.
In the middle of this chaos, the CDC's Get Smart About Antibiotics Week seemingly appeared out of nowhere and CDDEP investigators just published a very nice antibiotic use point prevalence study in 6 US hospitals in this month's Lancet ID to coincide with the 'Get Smart' Campaign. Nikolay Braykov and Dan Morgan led the study and Nikolay wrote up a nice post describing what they found, which I've excerpted below:
We undertook a chart review study at six institutions – two teaching centers, three community hospitals and one VA – looking at the indications for starting antimicrobials, the use of culture and radiology results and the patterns of modifying empiric therapy in the first five days of treatment. We found nearly two-thirds of inpatients were receiving antibiotics, with empiric starts dominated by combinations of vancomycin, piperacillin/tazobactam and fluoroquinolones. It is likely that a lot of those initial prescriptions were unnecessary, as 30% of patients lacked fever or abnormal white blood cell counts at the start.
In the middle of this chaos, the CDC's Get Smart About Antibiotics Week seemingly appeared out of nowhere and CDDEP investigators just published a very nice antibiotic use point prevalence study in 6 US hospitals in this month's Lancet ID to coincide with the 'Get Smart' Campaign. Nikolay Braykov and Dan Morgan led the study and Nikolay wrote up a nice post describing what they found, which I've excerpted below:
We undertook a chart review study at six institutions – two teaching centers, three community hospitals and one VA – looking at the indications for starting antimicrobials, the use of culture and radiology results and the patterns of modifying empiric therapy in the first five days of treatment. We found nearly two-thirds of inpatients were receiving antibiotics, with empiric starts dominated by combinations of vancomycin, piperacillin/tazobactam and fluoroquinolones. It is likely that a lot of those initial prescriptions were unnecessary, as 30% of patients lacked fever or abnormal white blood cell counts at the start.
Appropriate cultures (on
or before start of therapy) were collected from 59% of patients, and although 60%
came back negative, only 22% of all evaluated patients and had their
antibiotics narrowed or stopped (Figure). More specifically, 22/59 (37%) of patients with
negative urine culture and 11/22 (50%) of those with negative blood culture had
antimicrobials stopped or narrowed. Of pneumonia patients with negative chest
imaging that proportion was 12/50 (24%).
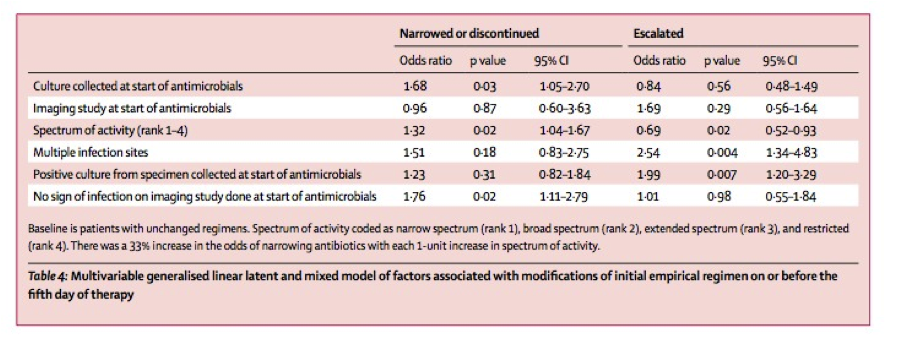
Narrowing or
discontinuation (of antibiotic therapy) was more likely when cultures were collected at the start of
therapy and no infection was noted on an initial radiological study. In turn,
escalation was associated with multiple infection sites and a positive culture
(see table below).
It seems like diagnostic uncertainty drives a
lot of possibly unnecessary antibiotic use. These results underscore not
only the need for rapid diagnostics, but also the importance
of mechanisms to assure tests are ordered in time and their results are actually
used to optimize therapy – goals attainable through better stewardship programs
and physician education.
A great point made recently is that the government’s resistance action plans should include steps to incentivize and expand the training of more ID physicians. Although the threat of drug resistance gets more public attention each year, “getting smart” about antibiotics, including their timely withdrawal and adjustment, ultimately requires the buy-in of current and future prescribers.
A great point made recently is that the government’s resistance action plans should include steps to incentivize and expand the training of more ID physicians. Although the threat of drug resistance gets more public attention each year, “getting smart” about antibiotics, including their timely withdrawal and adjustment, ultimately requires the buy-in of current and future prescribers.

Comments
Post a Comment
Thanks for submitting your comment to the Controversies blog. To reduce spam, all comments will be reviewed by the blog moderator prior to publishing. However, all legitimate comments will be published, whether they agree with or oppose the content of the post.